to OR or not to OR, that is the question
73 year old female presents with hypo-tension, found on routine BP check, with BP of 60/30. Patient is afebrile, and has a WBC count of 14,000. Lactate is 1.6 mmol/L, which is within normal limits. Abdomen is soft. Due to concern for sepsis, a CT scan of the abdomen is performed, which shows extensive penumatosis, with air extending into the SMV and portal vein. She is taken emergently to the OR, where on exploration, the surgeons find “diffuse small bowel dilation, adhesion’s, all bowel viable”.
This is benign pneumatosis, which we know occurs up to 30% of the time. Differentiating between benign pnematosis and ischemic bowel is very difficult. This paper talks about some of the CT signs that can differentiate between the two, and many others have looked at the shape of air in the bowel wall as a differentiating factor. This review in AJR concludes “There are many benign and life-threatening causes of PI. The imaging appearance of both may look very similar. Therefore, correlation with clinical history, physical examination, and laboratory test results is the best indicator of whether PI is due to a benign or life-threatening cause.”
Try convincing a surgeon to not operate on a case like this, with hypotension and leukocytosis, and the clinical correlation is always going to be difficult.
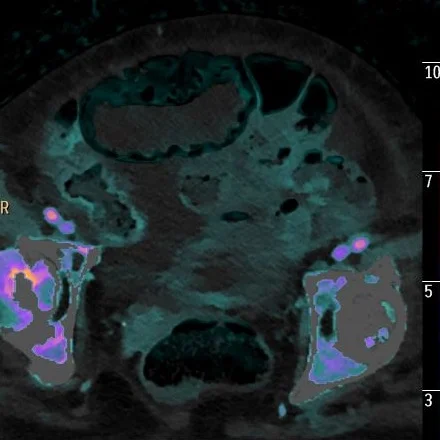
How about Spectral CT? Now, I am not saying that the course should have been different in this case, but that it could have been different. All the loops with pneumatosis have iodine uptake. This is nicely seen on iodine overlay, and the videos are uploaded on my twitter account (@ctspectral).
If we can avoid a patient like this from an unnecessary trip to the OR, we will be doing everyone a huge favor!
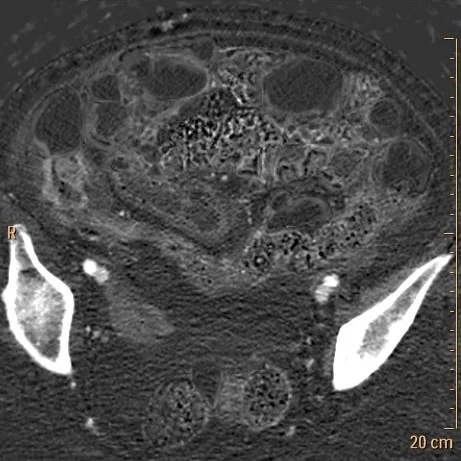
Conventional CT: Extensive pnematosis.
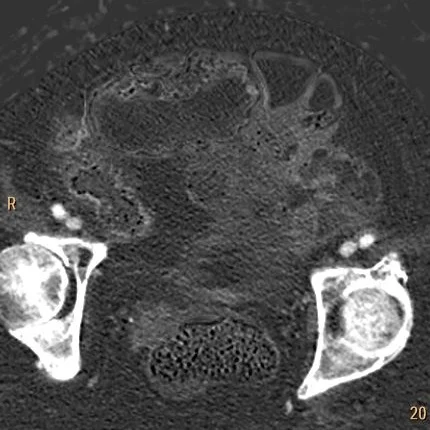
Iodine map: ALL of these loops have iodine uptake!
Iodine overlay: Nicely depicts perfusion to these loops.
Conventional CT: Note pnematosis in the dilate loop anteriorly.
Iodine map: There is perfusion!
Iodine overlay: Nicely depicts perfusion to these loops. We could have treated this conservatively.