Transient bowel ischemia
70 year old male with history of severe COPD and 3-vessel coronary artery disease, witnessed cardiac arrest in care facility. EMS got to him within less than 3 minutes and began CPR. He was in PEA and was never shocked. Within ~3 min of EMS chest compressions he had ROSC (return of spontaneous circulation) and was intubated in the field. A CT of the chest, abdomen and pelvis performed.
CT chest shows severe COPD. CT abdomen showed mesenteric venous air and pnematosis. On spectral analysis, there are several scattered small bowel loops with absent iodine uptake. Mesenteric vessels were widely patent. The ED was called, non-occlusive mesenteric ischemia was suspected. Lactate came back high (4.7, normal is 0.7 - 2.1 mmol/L).
But it did not make sense to my friend the ED doc. He was down for a very short time!
I stuck to my guns, I have to trust my images. The patient was taken to the OR later that evening. After several hours of painstaking dissection of extensive adhesions, all bowel was viable. There was NO bowel ischemia.
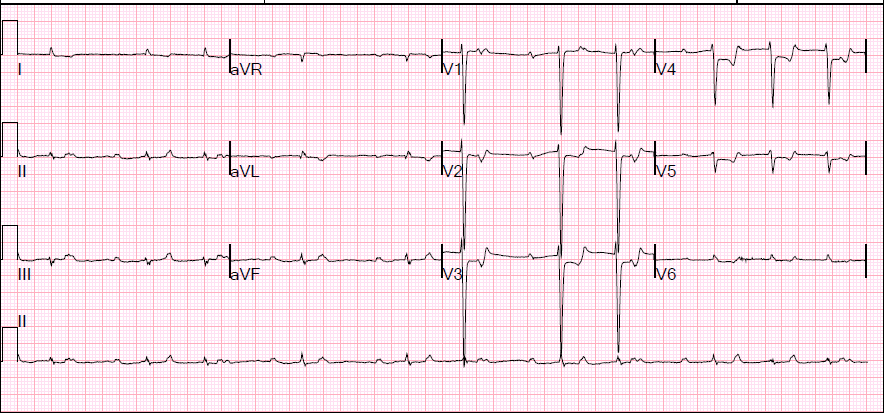
I was wrong, and my ED doc was right. Dr Steve Dunlop, being very kind, suggested that I was right too. It is very common to see extensive subendocardial ischemia after CPR. Perhaps, he suggested, the small bowel findings were analogous to findings in the heart?
So I check the EKG. This patient had very extensive ST depressions at presentation. These completely normalized on the next EKG done 40 minutes later. I could not find any definite descriptions of this entity in the literature, but I think what you see here is transient bowel ischemia after cardiac arrest and CPR, with pneumatosis, mesenteric venous gas and absent perfusion on the initial CT that nomalized by the time patient was taken to the OR.
It may be worthwhile to consider observation rather than jump to intervention in these cases.
Chest CT shows severe COPD
Conventional CT shows mesenteric venous air (red arrow)
Conventional CT with multiple foci of pnematosis (red arrow)
Iodine map: Cluster of loops in anterior abdomen without iodine uptake (blue oval)
Iodine map: A second loop in left upper quadrant without perfusion
First EKG: Note extensive ST depressions (most marked in V2-V6)
Second EKG (40 minutes later): The ST depressions have normalized!